Getting support for sexual problems
Help and support for sexual problems after treatment for prostate cancer.
Some treatments for prostate cancer will cause problems with sexual function.
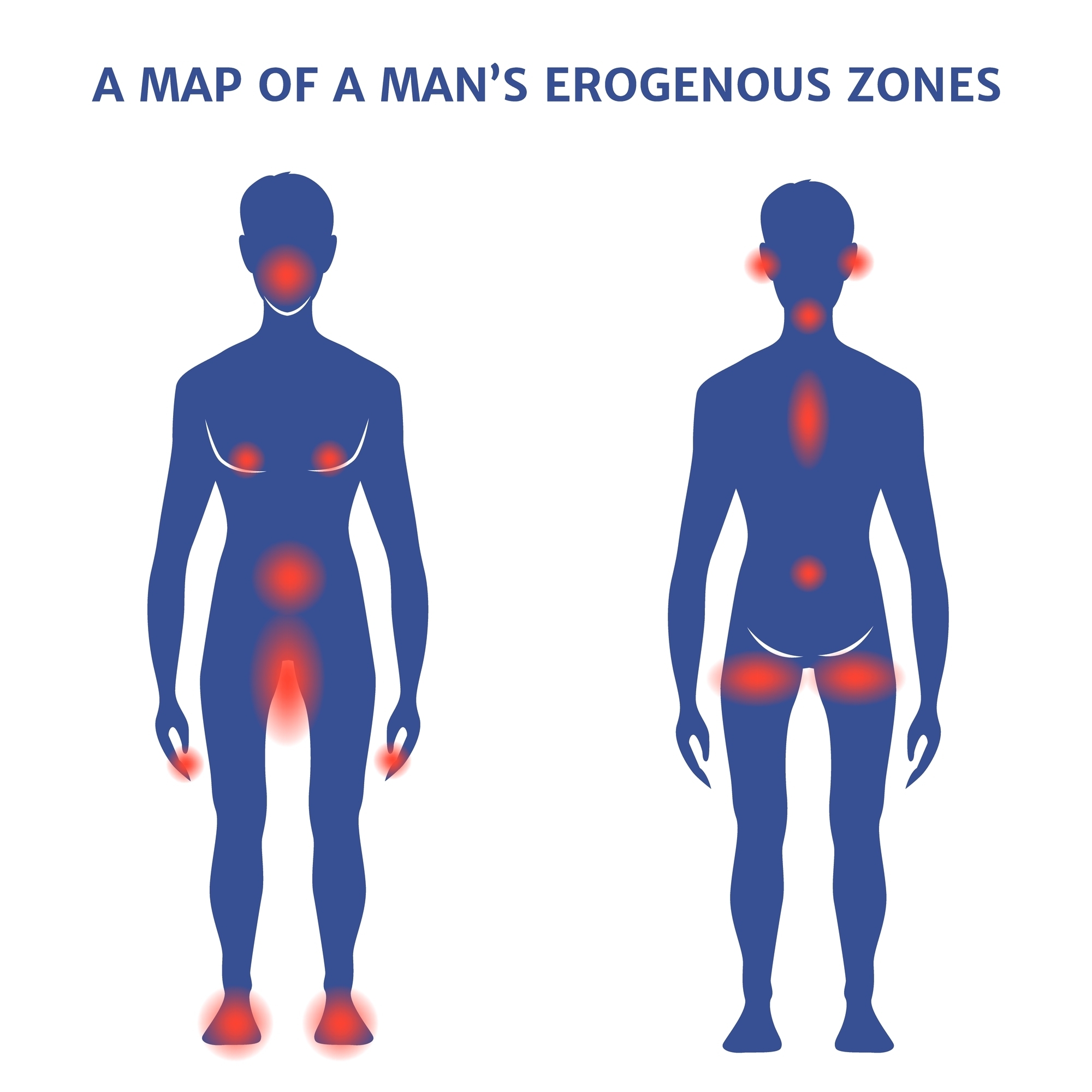
These problems include:

Getting or keeping an erection (erectile dysfunction)

Dry ejaculations

Reduced penis size

Loss of sexual interest

Problems with orgasms
Pain during or after receptive anal sex (anodysparunia)
NICE provides guidance on:
Learn more about NICE and what they do by visiting their website (this link will open in a new tab).
NICE has put together guidelines for the diagnosis and management of prostate cancer.
Please note that these are just guidelines and are not a legal requirement.
You can use this information to help you to ask questions of your healthcare team.

Tell you about the risk of dry orgasms and fertility issues after some treatments for prostate cancer. This should happen before you make your treatment decision.

Offer you the chance to freeze your sperm.
You can learn more about sperm banking from the Human Fertilisation and Embryology Authority (HFEA). You can visit HFEA’s website here (this will open an external tab).
Cancer Research UK (CRUK) also have information about sperm collection and storage on their website. You can visit CRUK’s website here (this will open an external tab).

Access to specialist services that can help you.

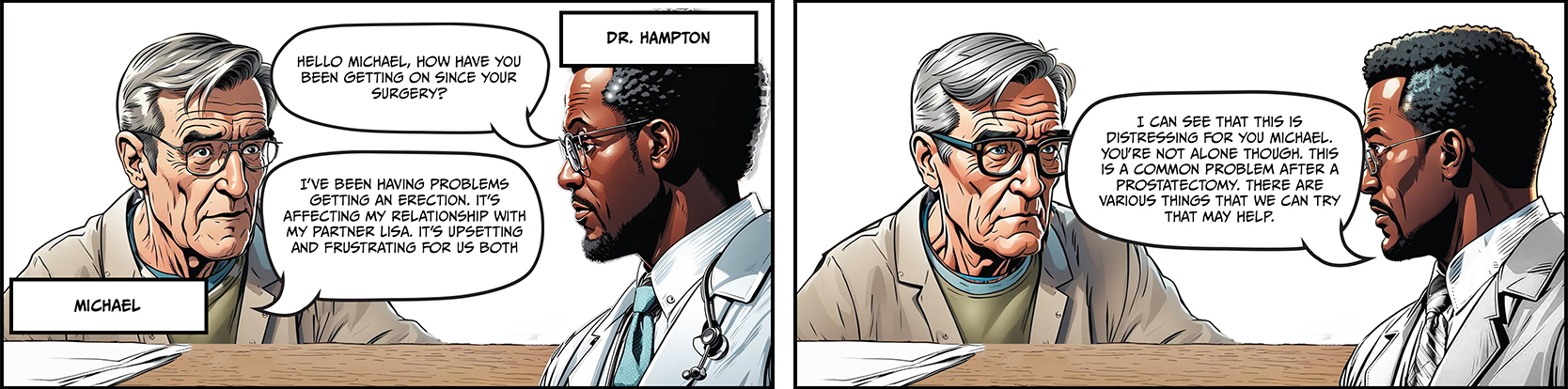
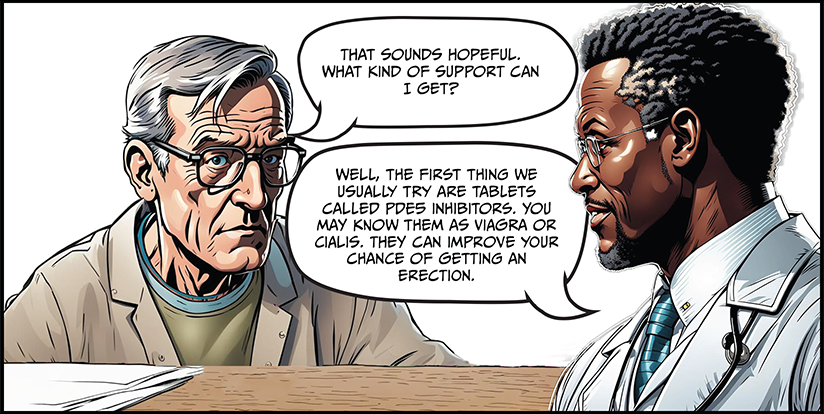
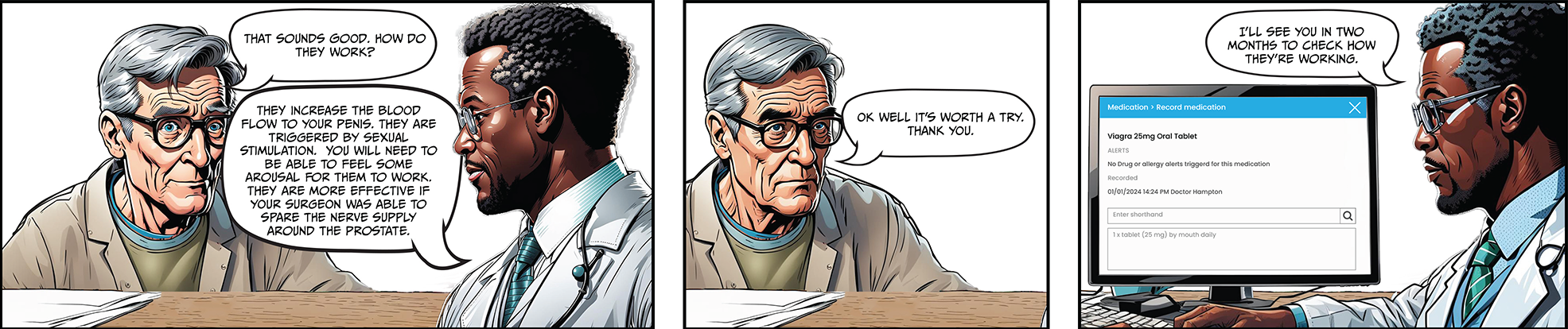
Medication called PDE5 inhibitors (for example, Viagra or Cialis).
You should also be offered the chance to talk to a psychosexual therapist.

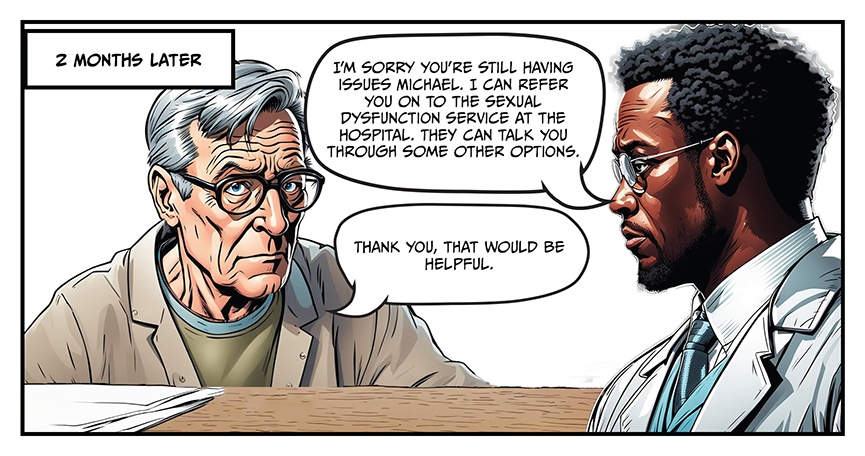
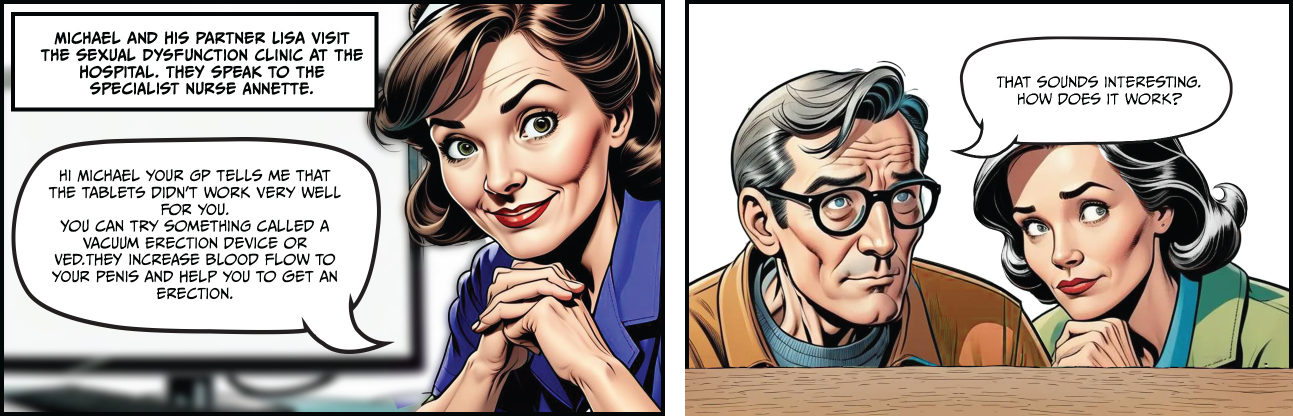
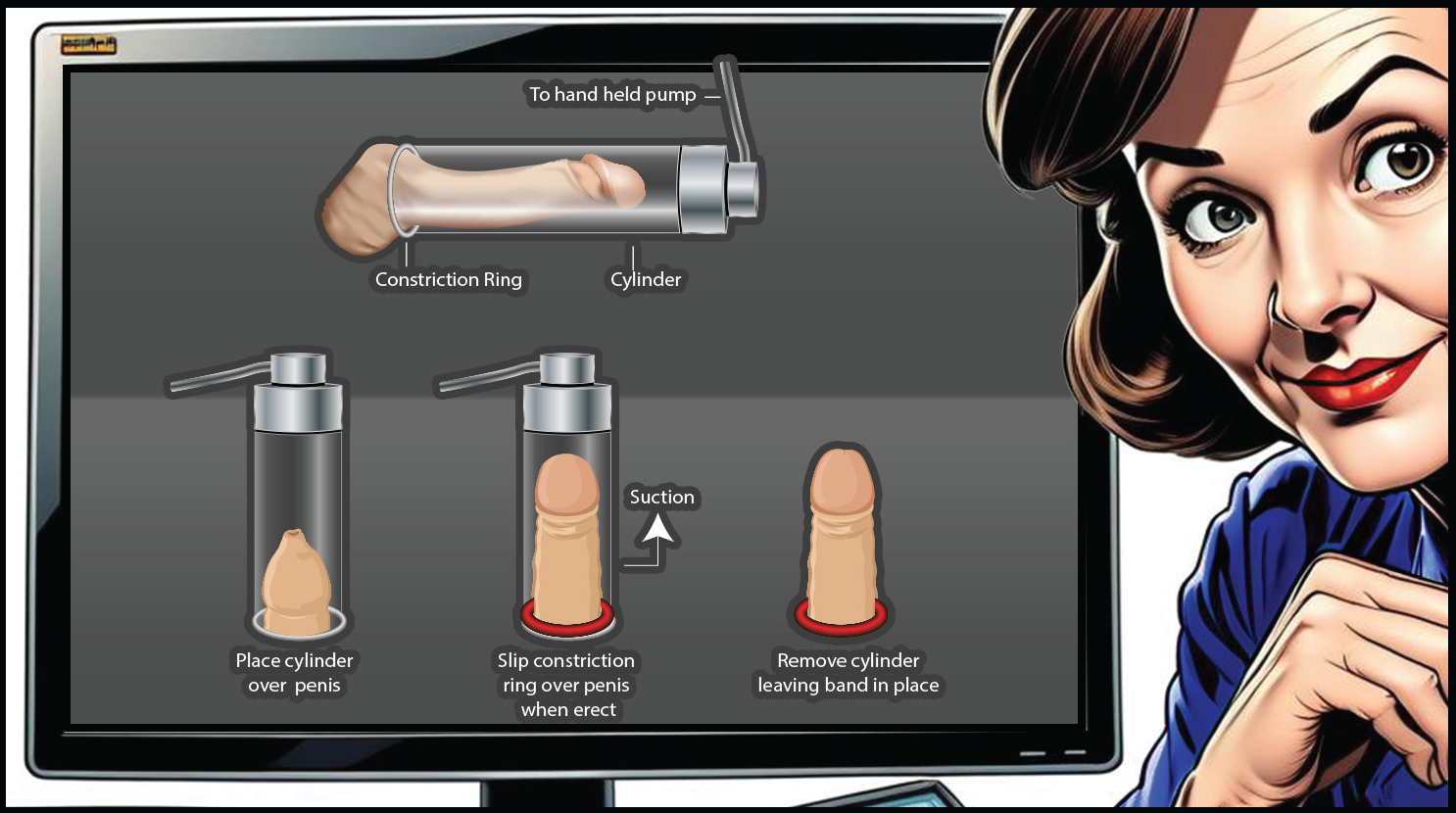
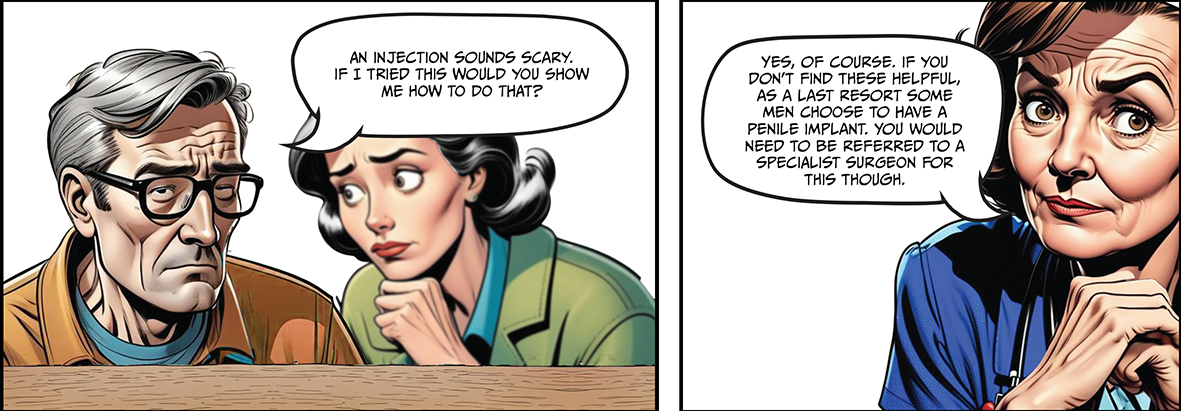
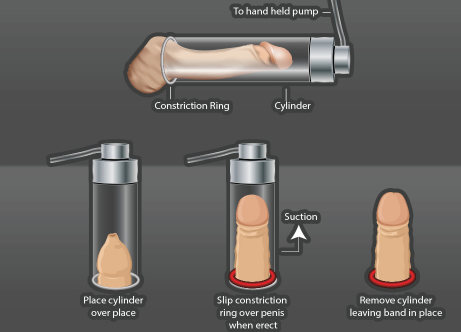
The following cartoon strip shows the different options available to you if you have problems getting an erection.
You can read the leaflet from the British Association of Urological Surgeons (BAUS) for more information about VEDs and how to use them. This is a PDF document and may not be compatible with screen readers. Listen to the PDF on VEDs
An ICB is also responsible for:
You can ask them:
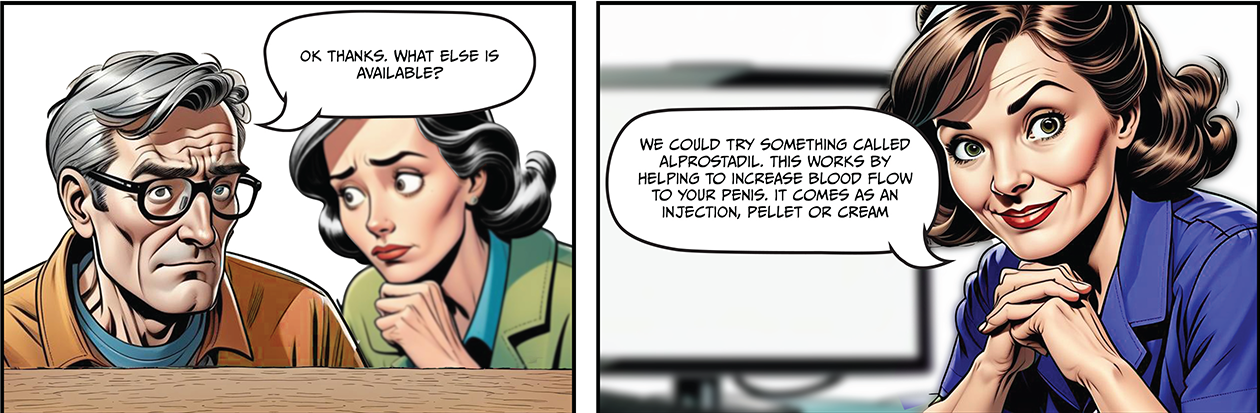
CREAM (VITAROS)

PELLETS (MUSE)
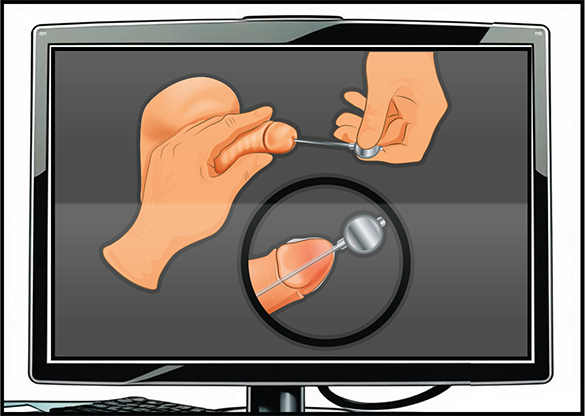
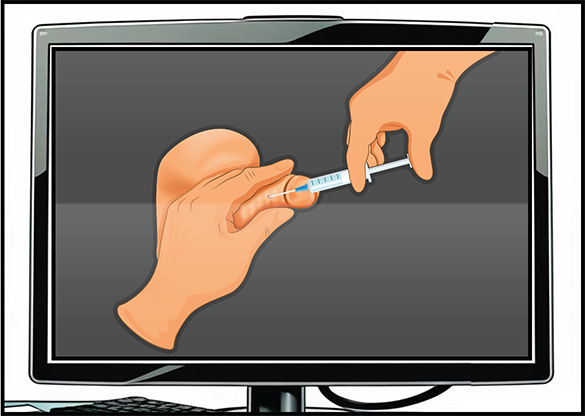
INJECTION (CAVERJET)
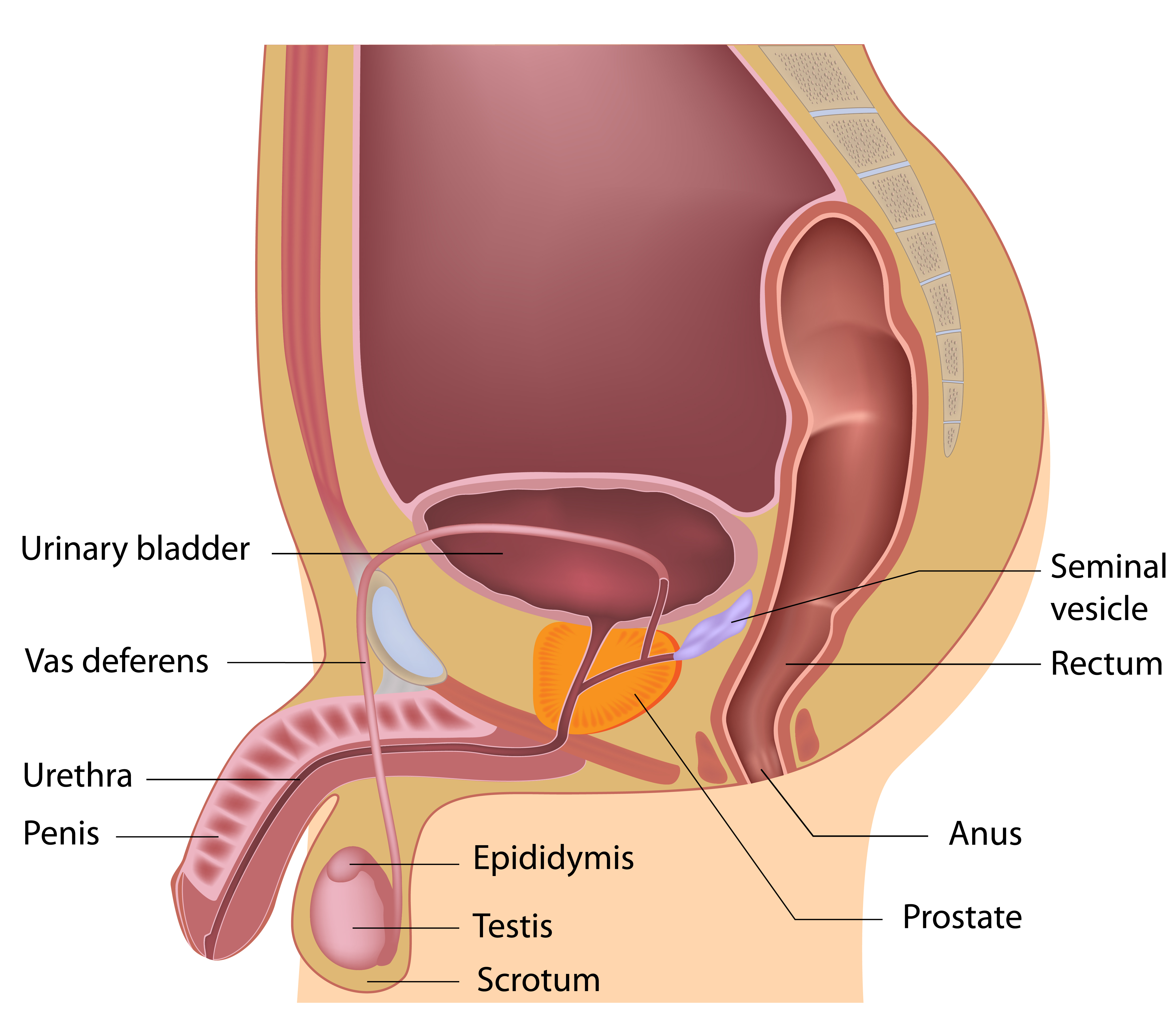
 Dry ejaculations after radical prostatectomy
Dry ejaculations after radical prostatectomy Dry ejaculations after external beam radiotherapy
Dry ejaculations after external beam radiotherapy Dry ejaculations after brachytherapy
Dry ejaculations after brachytherapy Dry ejaculations whilst on hormone therapy
Dry ejaculations whilst on hormone therapy





The use of a vacuum erection device may also help to increase blood flow.

PSA test
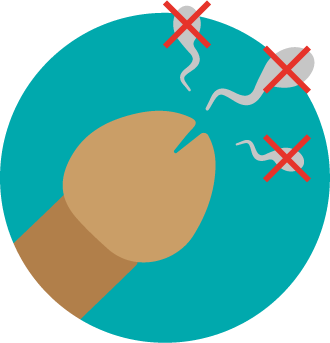
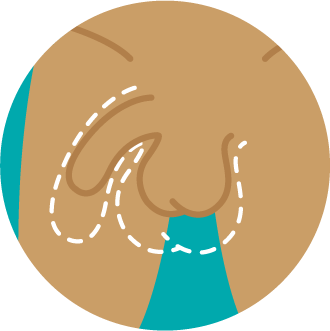
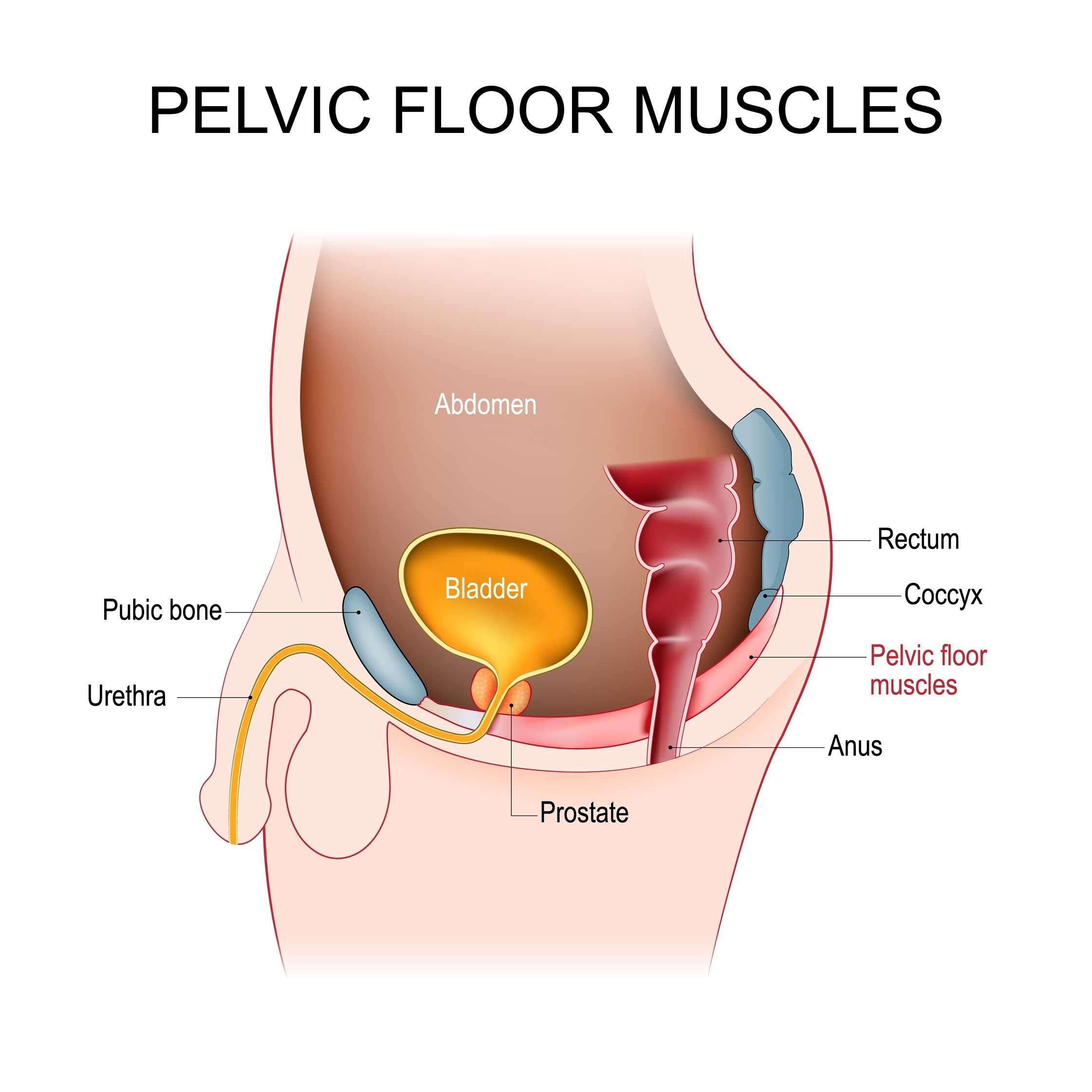
If you still have a prostate, avoid anal sex for one week before a PSA test. Prostate massage can increase PSA levels.

Prostate biopsy
Avoid anal sex for two weeks following a transrectal prostate biopsy. This allows the skin in your rectum to heal properly. This will decrease the chance of infection.
Avoid anal sex for one week after a transperineal prostate biopsy. This allows the skin to heal and any bruising to calm down. Allowing time to heal will reduce the chance of painful sex.

Radical prostatectomy
If you have had a radical prostatectomy wait for six weeks before having anal sex. You need to wait for internal healing to happen. Having anal sex before this time may make peeing problems (urinary incontinence) worse.

External beam radiotherapy
If you have had external beam radiotherapy, you should wait about two months before having anal sex. The rectal skin will be inflammed and more prone to damage.

High-dose rate (temporary) brachytherapy
If you have had high-dose rate (temporary) brachytherapy, you should wait two months before having anal sex. This will give time for any rectal inflammation to settle.

Low-dose rate (permanent seed) brachytherapy
If you have had low-dose rate (permanent seed) brachytherapy, you should wait about six months. This allows for rectal inflammation to heal. This also reduces the radiation to your partner's penis during anal sex.







Have a conversation with your healthcare team about your fears around possible changes to your sex-life and relationships before you decide on a treatment.


David's partner has had surgery for prostate cancer. Listen to him quiz therapist Andy about the issues he and his partner are experiencing since the surgery.
They talk about dealing with:
Therapist Andy is a member of the College of Sexual and Relationship Therapists. Visit their 'find a therapist' page (link will open in a new tab) to look for a therapist near you.
The toolkit is an information resource for people affected by prostate cancer. The development has been funded through an educational grant from Advanced Accelerator Applications (A Novartis Company).

In 2021 Prostate Cancer Research, in collaboration with Tackle Prostate Cancer, developed a webinar series Living Well with Prostate Cancer. We have two webinars dealing with sex and intimacy.
2. Sex and intimacy - LGBTQ community
They also provide information for partners.

The toolkit is an information resource for people affected by prostate cancer. The development has been funded through an educational grant from Advanced Accelerator Applications (A Novartis Company).