Radical Prostatectomy (Surgery)
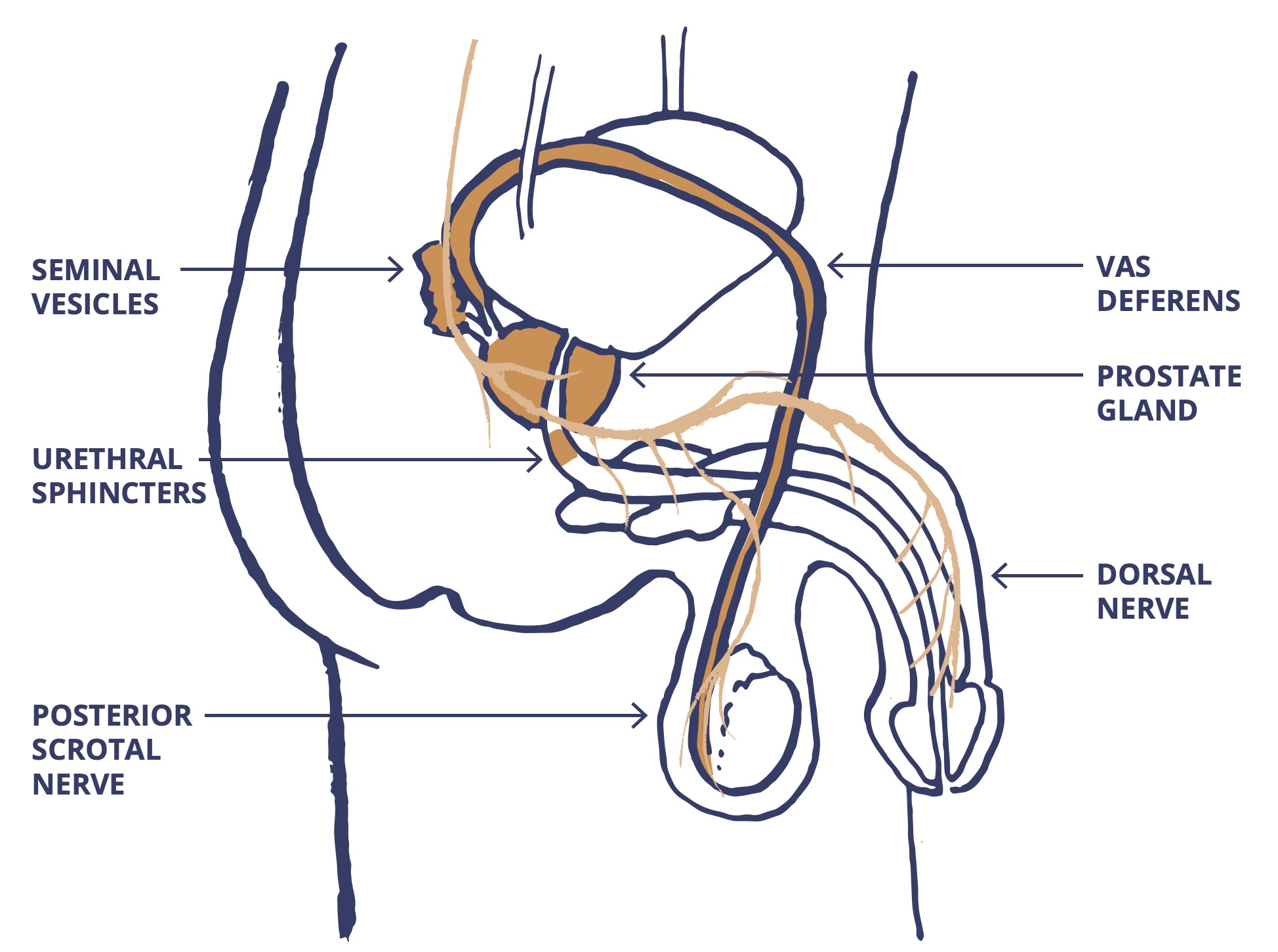
The surgical removal of your prostate gland, the cancer inside it, the internal urinary sphincter and the seminal vesicles.
Watch our short animation to learn more about radical prostatectomy.
You can have a radical prostatectomy if:
Your cancer has spread to the area just outside of the prostate (locally advanced).
You cannot have a radical prostatectomy If you have other health conditions such as:
Speak to your doctor about any other health conditions you have.
The surgeon will take out:
There are nerves and blood vessels around your prostate. These nerves help you to get an erection. The surgeon can operate in a way that will protect them. But, if your cancer has spread into these nerves or the area around the prostate, they may remove some or all of these nerves.
Talk to your surgeon about the possible effects of surgery on your erections. You can ask:
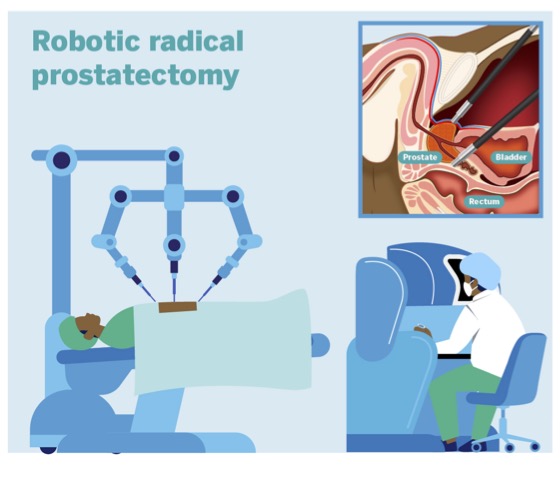
Radical prostatectomy can be carried out as:
You will be asked to come along to a pre-assessment clinic one-to-two weeks before your surgery. This will be at the hospital where you will be having your surgery. You will:
You will be asked to empty your bowel on the morning of your surgery. So, you may be given a small enema to use. An enema puts a small amount of fluid into your rectum. This helps to clear out your bowel. You can do this yourself.

You will be shown how to do exercises to strengthen your pelvic floor muscles. This can help reduce leakage of pee after the surgery. It is a good idea to start these before your surgery. Ask your healthcare team about pelvic floor exercises.
Visit our page on peeing problems to learn more about the pelvic floor.
Australian physiotherapist Michelle Kenway has put together a video called ‘Kegel Exercises for Men – Beginners Pelvic Floor Strengthening Guide' (this link will open in a new tab).

You will be visited by your surgeon who will:
You will also be seen by your anaesthetist who will ask you questions about:
You may be asked to wear a pair of compression stockings. These are sometimes called TED stockings. You may also have a heparin injection. This helps to thin your blood. Both help to stop blood clots (deep vein thromboses) forming in your lower legs.

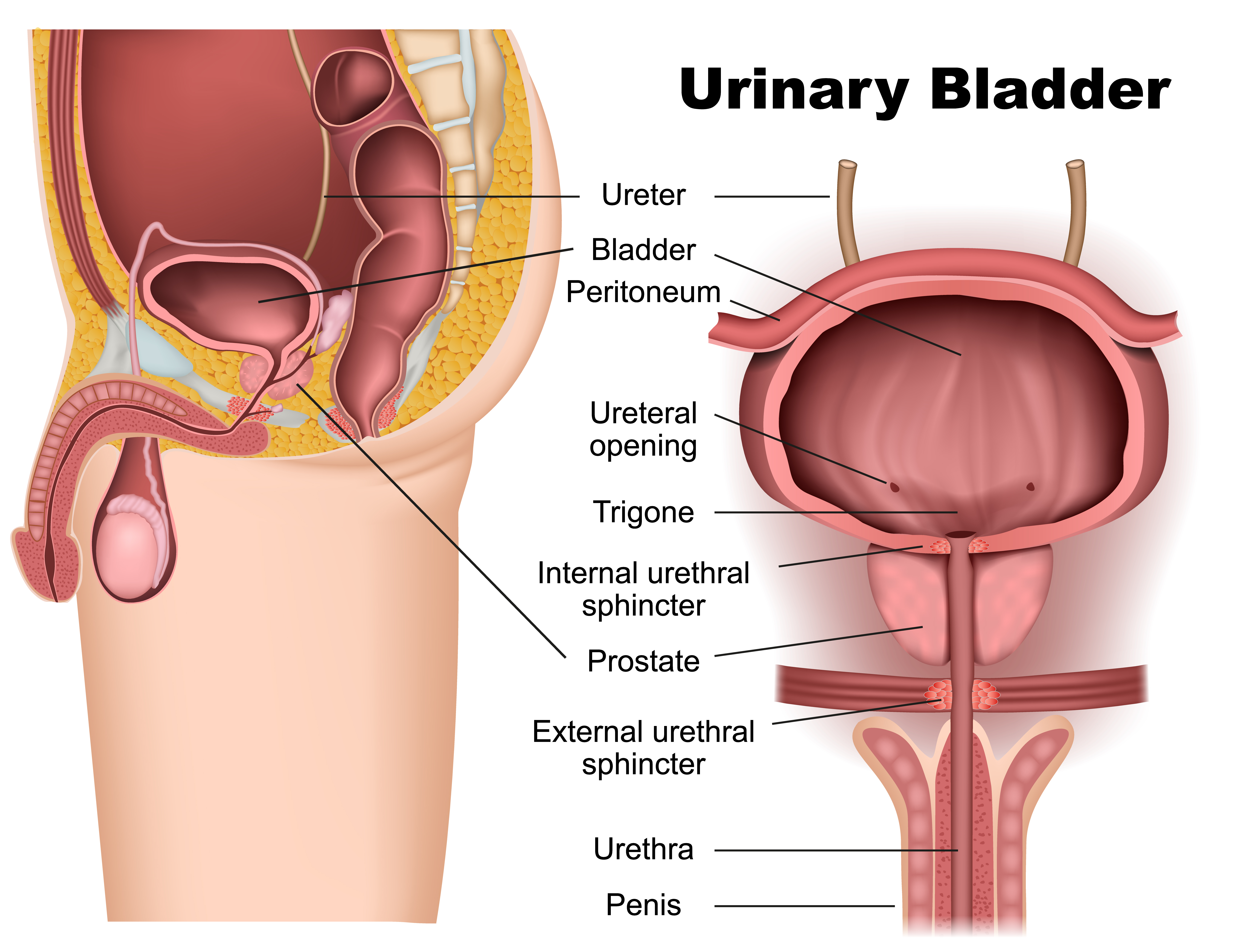
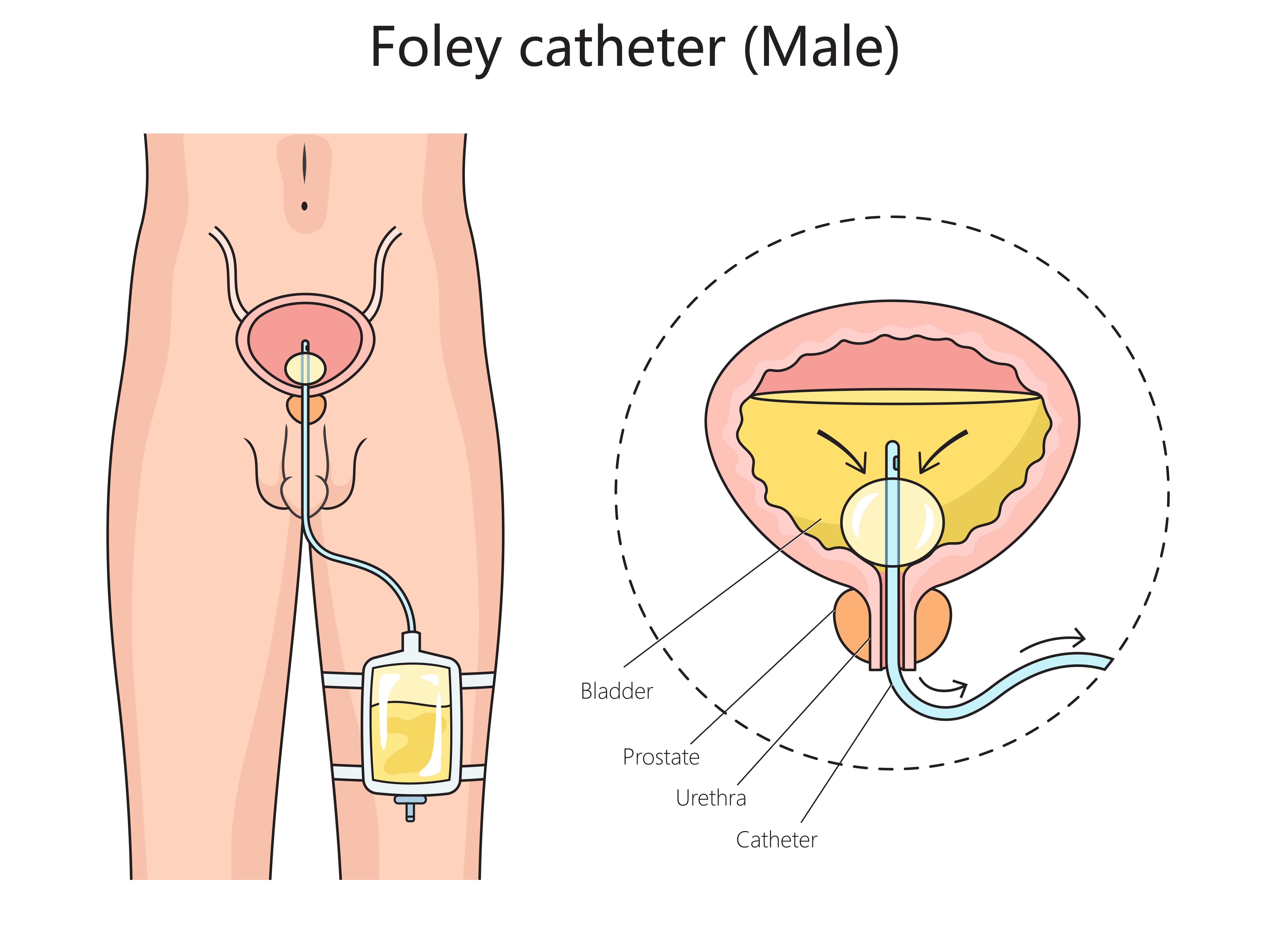
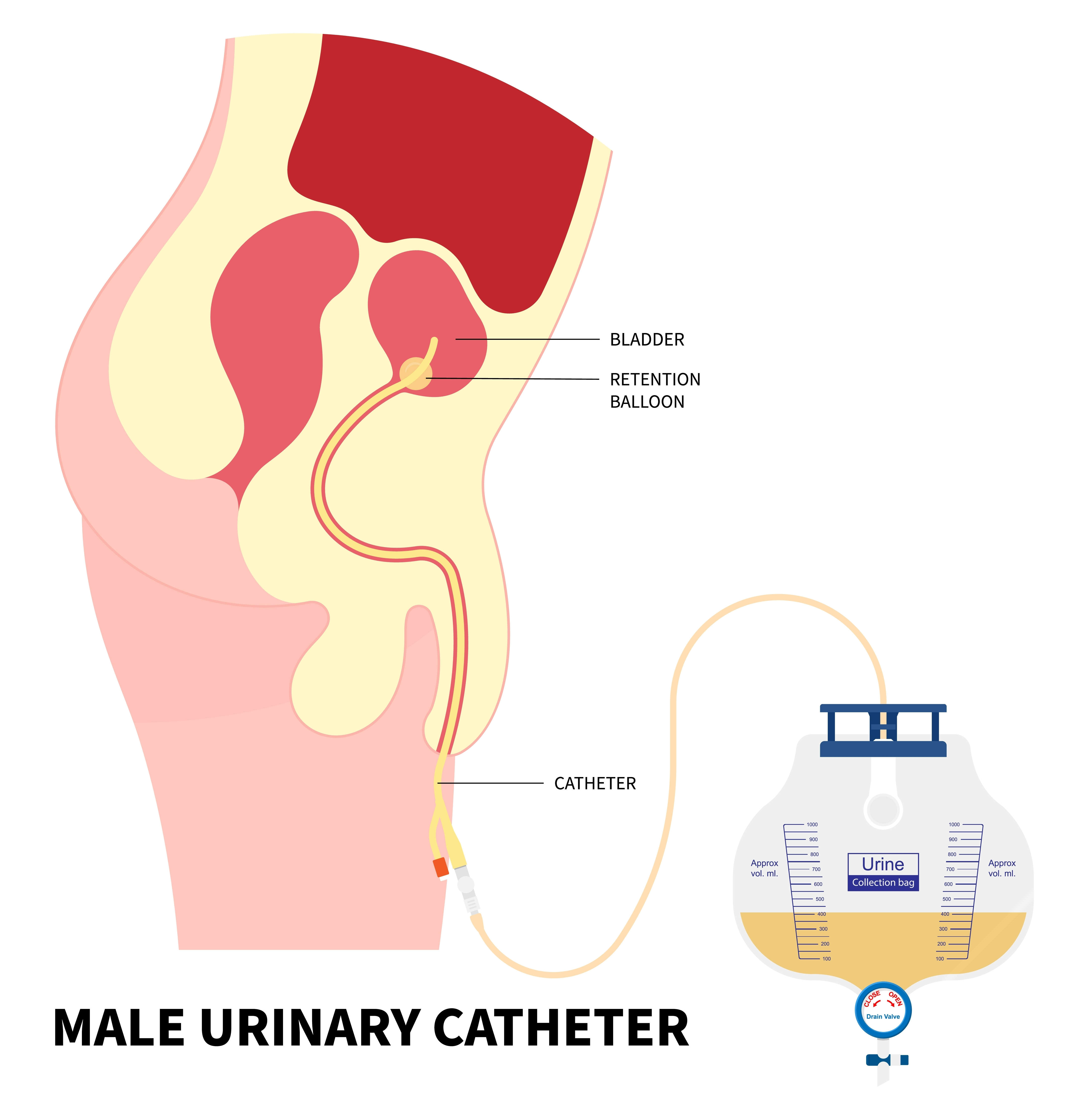
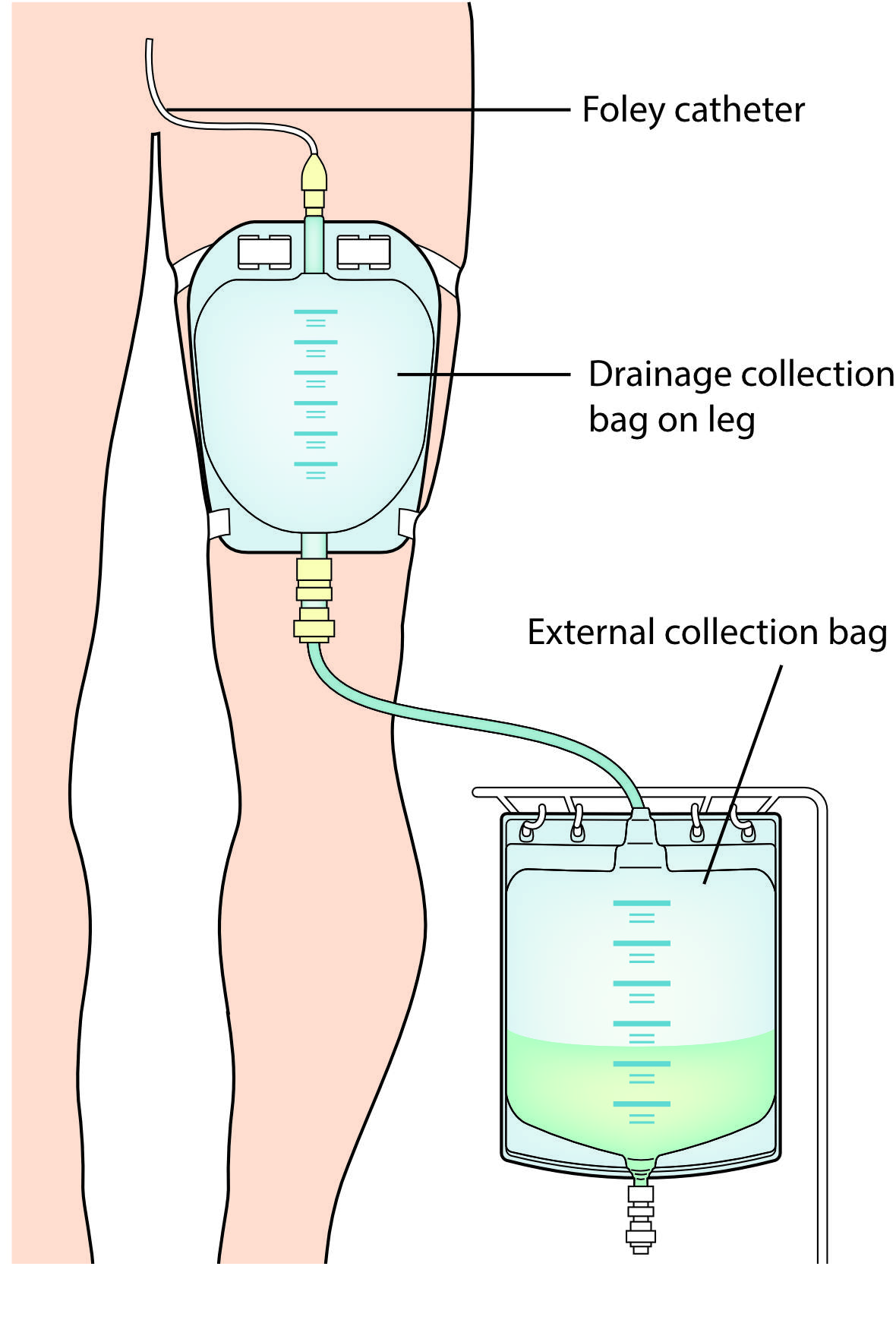
You will have a tube to drain pee from your bladder into a bag. This is called a urinary catheter.
You may get:
Pain will vary between people. It will also depend on what type of operation you have. Your healthcare team will give you advice on how to manage this.


This could be:

Radiotherapy on its own (salvage radiotherapy).

Hormone therapy injections and regular monitoring.

Always talk to your healthcare team if you are worried about side effects.


An indwelling catheter is a soft, flexible tube that is inserted into your bladder via your urethra (the tube that carries pee from your bladder to the outside).





If nothing works or you are experiencing pain, contact your healthcare team straight away. Remember to ask for an emergency contact before you leave hospital.
Listen to Urologist Marcus, quizzing radical prostatectomy patient Denzil, about his experience of having surgery for prostate cancer.

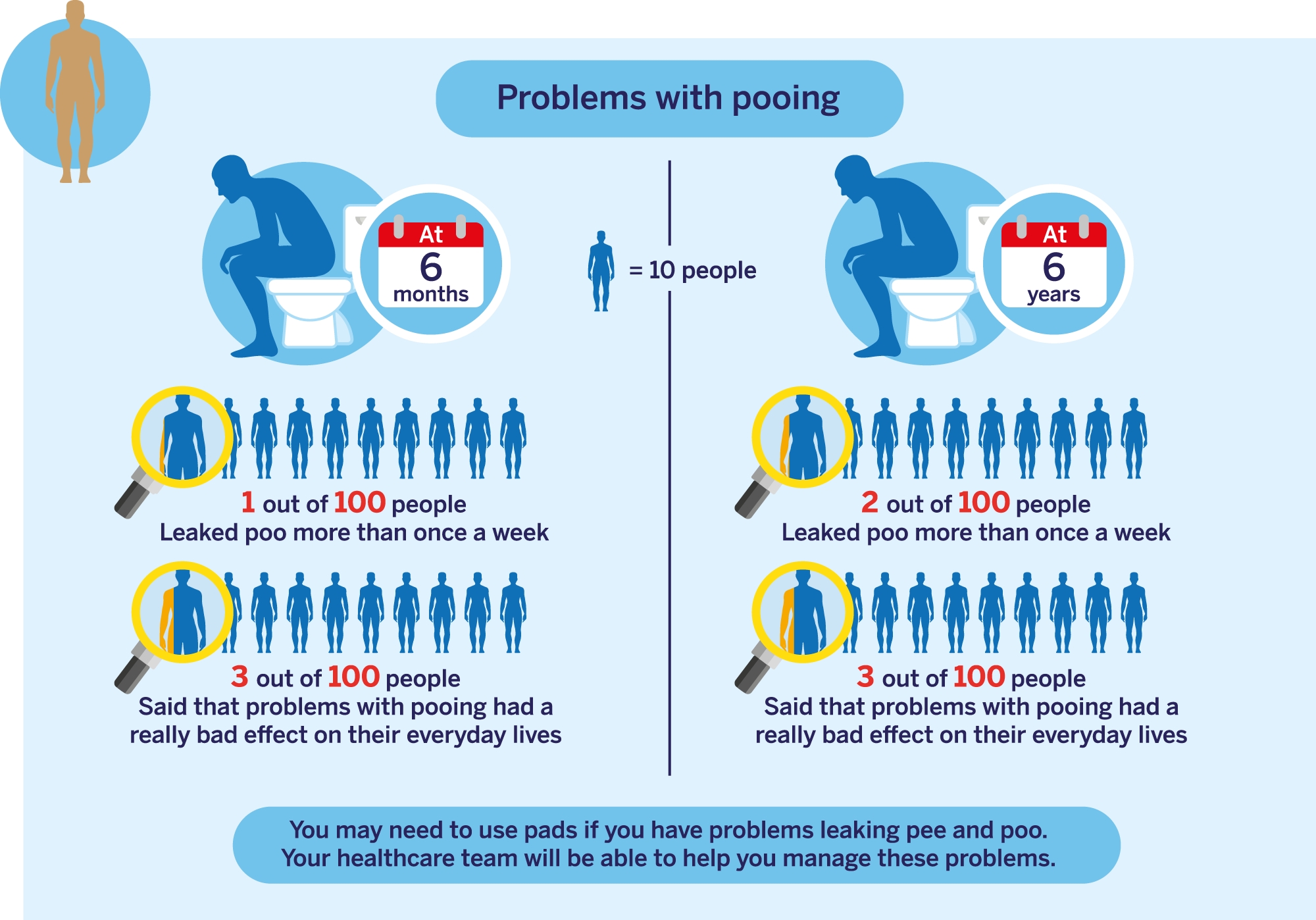
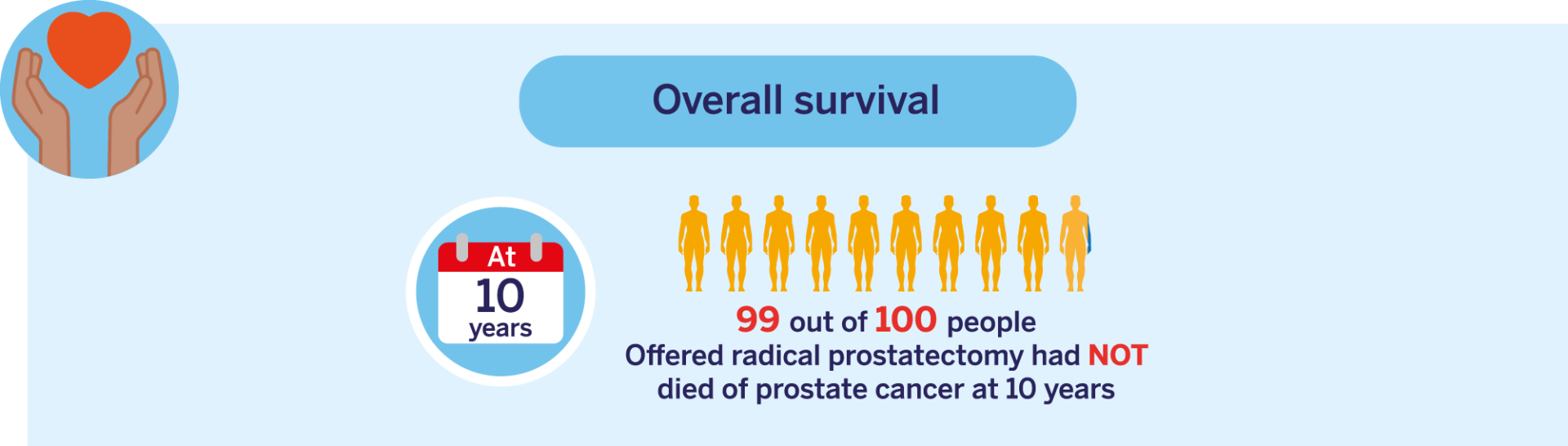
This data is for people with CPG 1, 2 and 3 localised prostate cancer. Click here to learn more about CPG groups (this will open in a new tab).
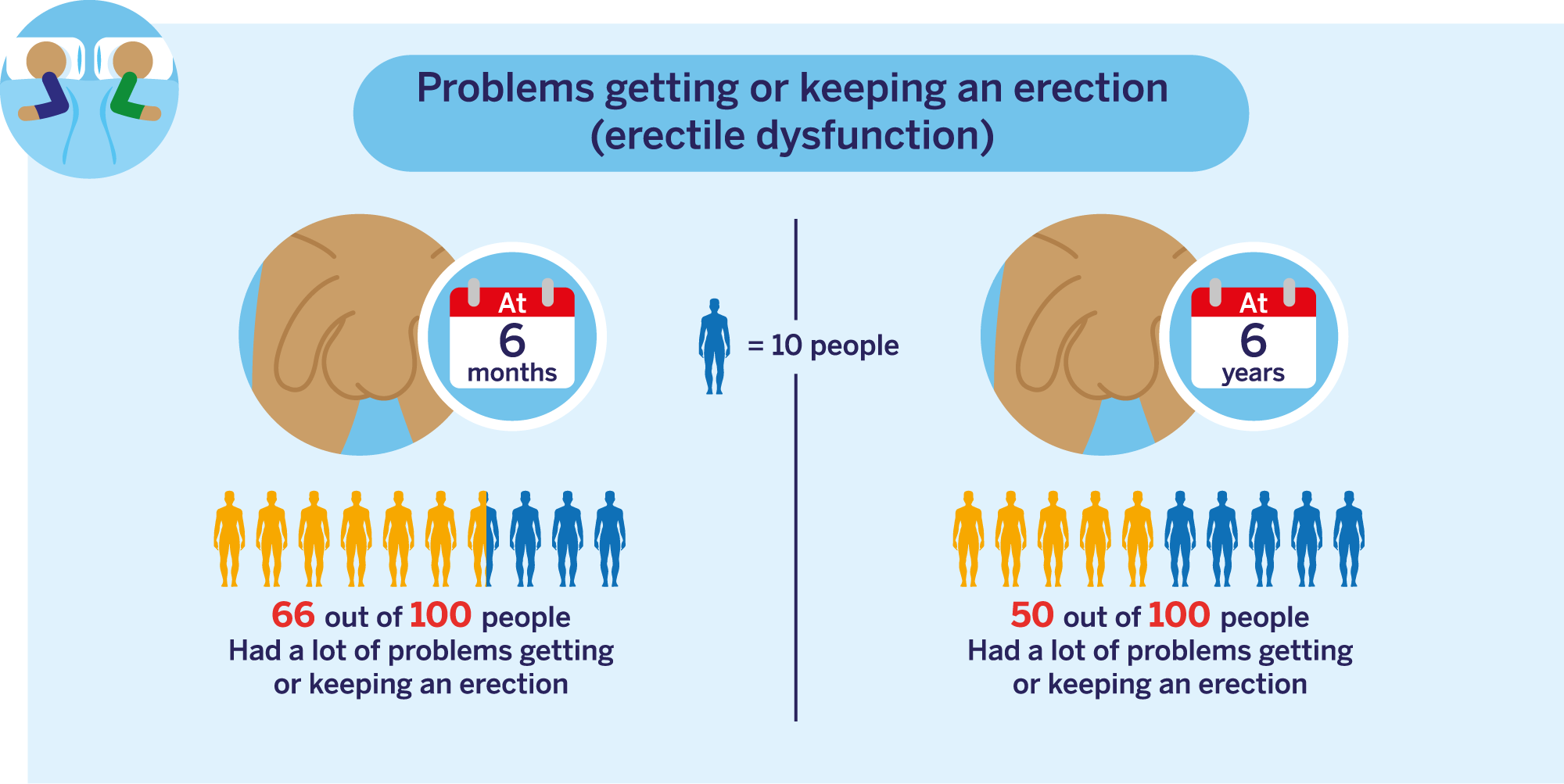
This data is for people with CPG 1, 2 and 3 localised prostate cancer. Click here to learn more about CPG groups (this will open in a new tab).
Enjoying activities such as walking or going out to the pub
70 out of 100
Ability to make good connections with others
60 out of 100
Ability to reach sexual arousal, either physically or emotionally
85 out of 100
Knowing who you are and what motivates you
67 out of 100
Feeling good and functioning well in your personal and professional life
68 out of 100
Ability to think clearly, make good decisions, and cope with your emotions
64 out of 100
Feeling of constant physical and/or mental tiredness or weakness
65 out of 100