Hormone Therapy (injections and relugolix tablets)
Injections or tablets that block or lower the amount of testosterone in the body. Also known as androgen deprivation therapy (ADT).
Watch our short video to learn more about hormone therapy.
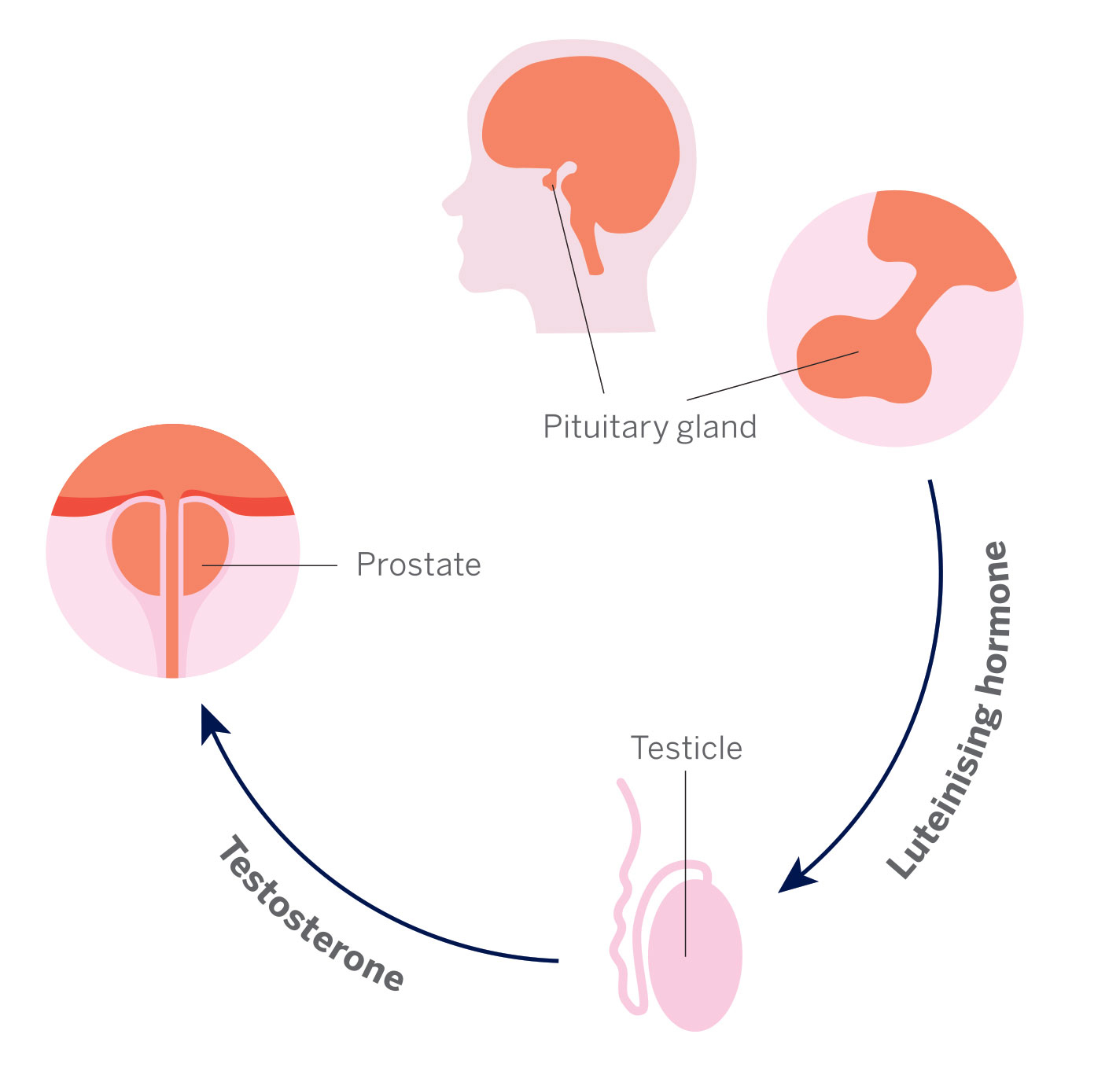
Growth and development of male sexual organs at puberty.
Relugolix (Orgovyx)
Degarelix acetate (Degarelix Ferring - previously called Firmagon)

As a treatment on its own. This may happen if you are not able to have radiotherapy or surgery. You may also have regular monitoring.
You may have your first injection at the hospital. But often it is done in your GP surgery. All of your follow-up injections will usually be done at your GP surgery.


 You will have regular check-ups with your doctor or specialist nurse.
You will have regular check-ups with your doctor or specialist nurse.
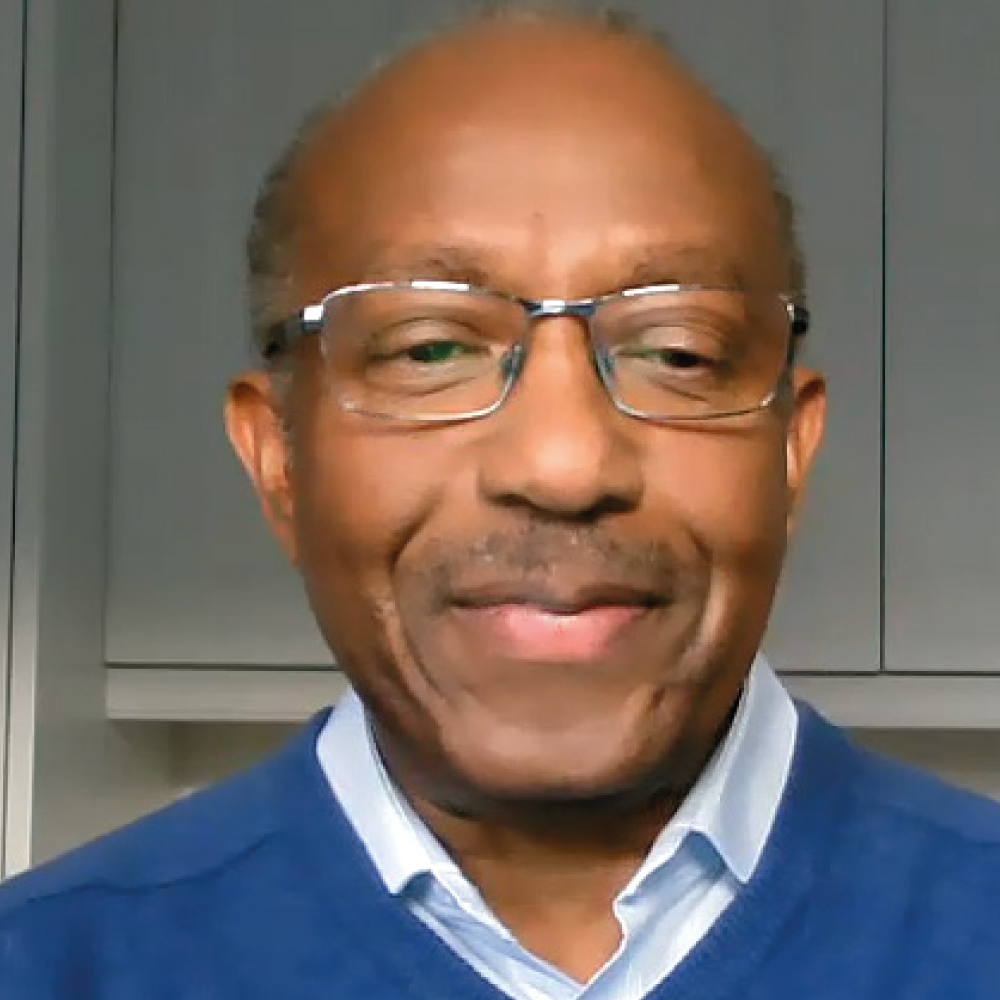
Listen to patient Clem speak to urology advanced nurse practitioner Kelly about his experience of having hormone therapy injections for his prostate cancer.

Enjoying activities such as walking or going out to the pub
86 out of 100
Ability to make good connections with others
56 out of 100
Ability to reach sexual arousal, either physically or emotionally
78 out of 100
Knowing who you are and what motivates you
73 out of 100
Feeling good and functioning well in your personal and professional life
77 out of 100
Ability to think clearly, make good decisions, and cope with your emotions
72 out of 100
Feeling of constant physical and/or mental tiredness or weakness
89 out of 100