Radiotherapy
External beam radiotherapy is a type of radiotherapy that is given from outside the body.
You can have EBRT if:
As cancer cells are not able to repair themselves very well radiotherapy can stop them from growing.

Visit the Cancer Research UK website (this link will open in a new external tab) for more detailed information about each type.
Radiotherapy machines


The radiotherapy treatment is painless.
Take a look at our page on hormone therapy to find out more. This link will open in a new tab.


Our services search tool (this link will open in a new tab) will allow you to search for hospitals near you that offer external beam radiotherapy.
Listen to patient Nick speak to Oncologist David about his experience of having radiotherapy for his prostate cancer.

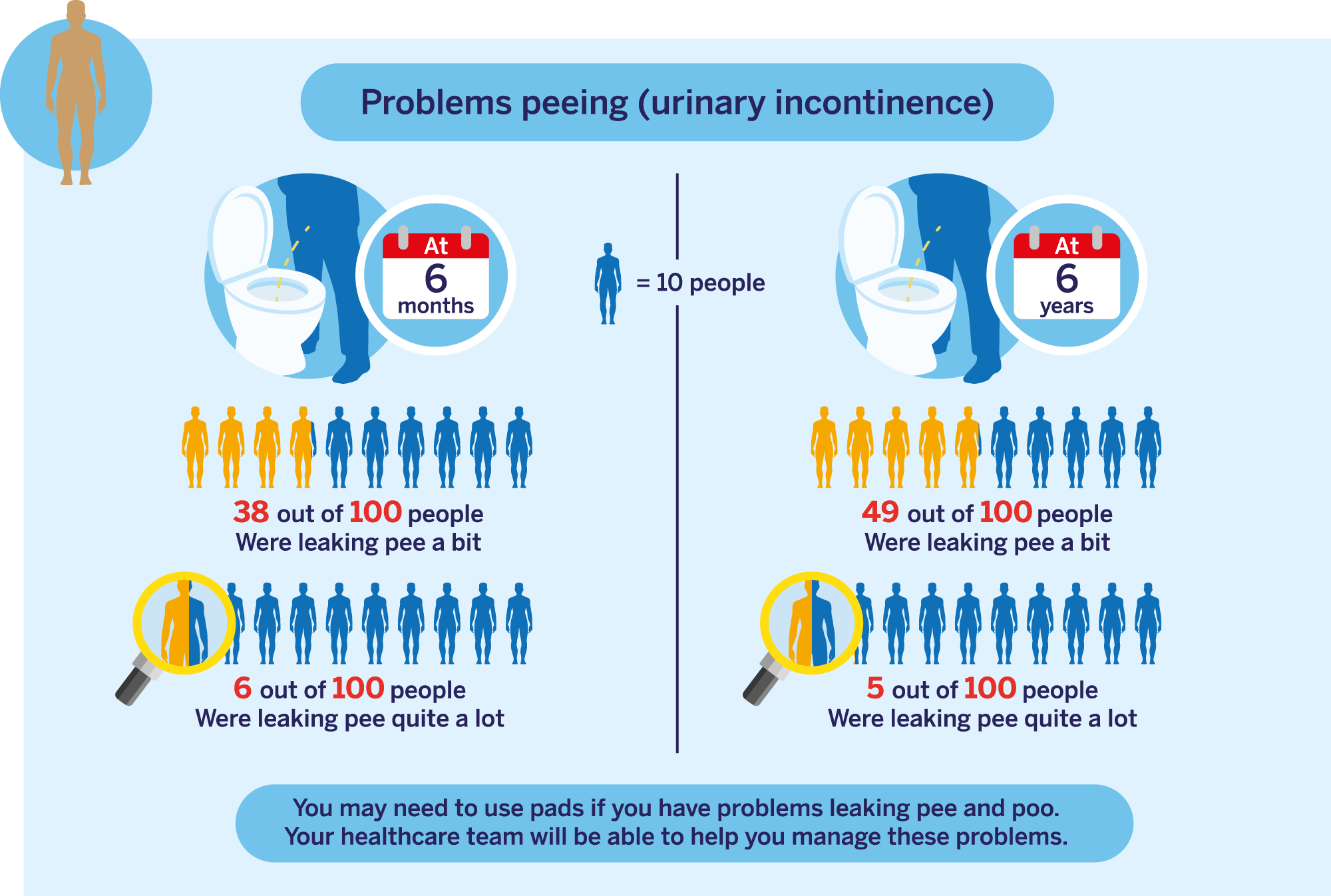
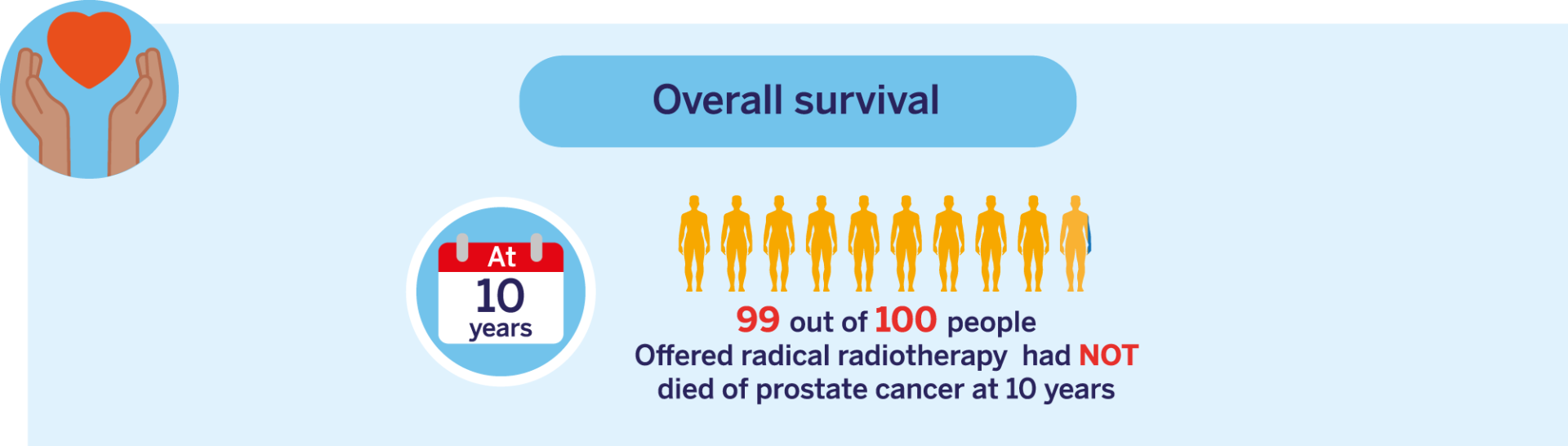
This data is for people with CPG 1, 2 and 3 localised prostate cancer. Click here to learn more about CPG groups (this will open in a new tab).
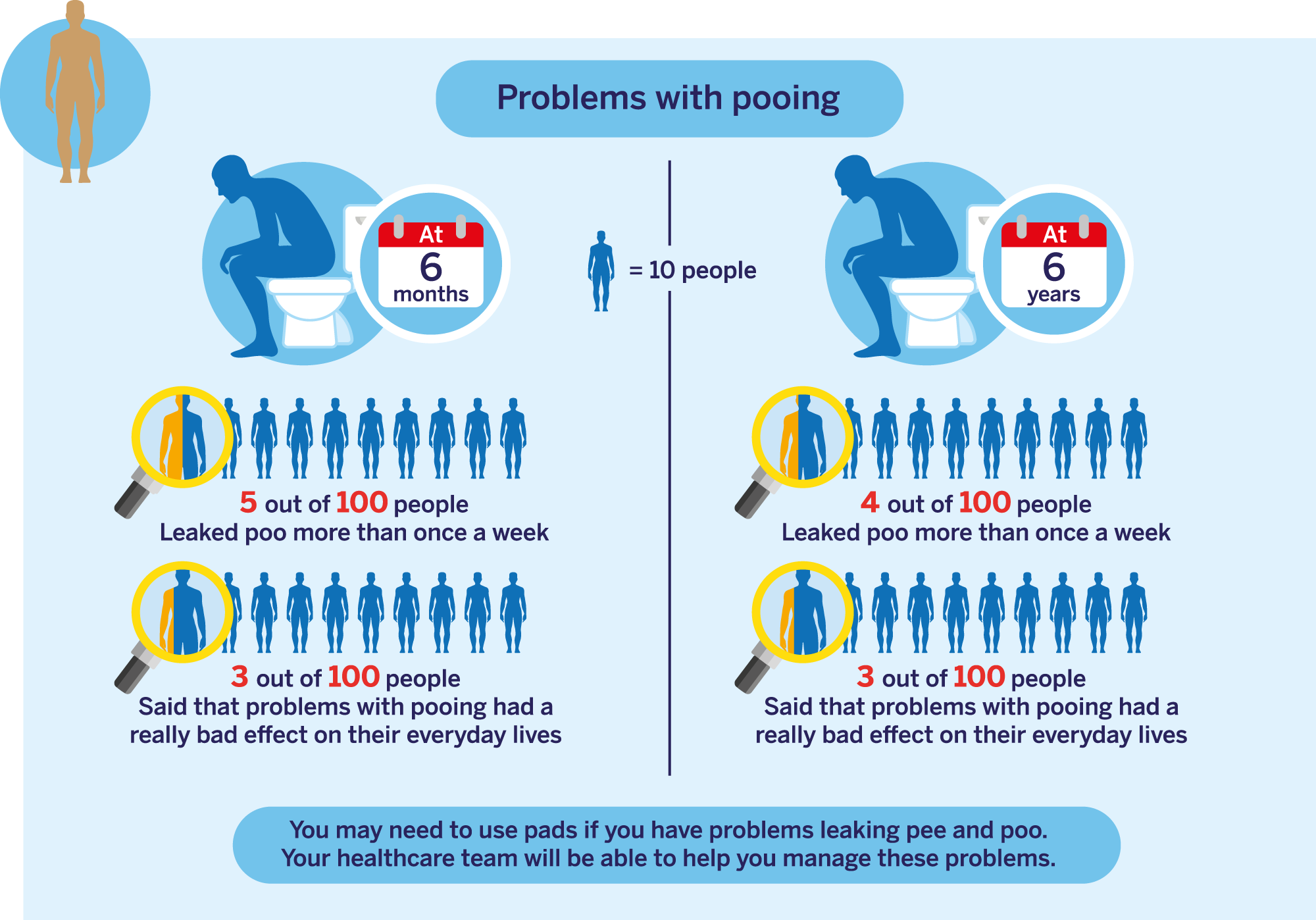
This data is for people with CPG 1, 2 and 3 localised prostate cancer. Click here to learn more about CPG groups (this will open in a new tab).
Enjoying activities such as walking or going out to the pub
76 out of 100
Ability to make good connections with others
56 out of 100
Ability to reach sexual arousal, either physically or emotionally
71 out of 100
Knowing who you are and what motivates you
60 out of 100
Feeling good and functioning well in your personal and professional life
66 out of 100
Ability to think clearly, make good decisions, and cope with your emotions
65 out of 100
Feeling of constant physical and/or mental tiredness or weakness
81 out of 100