Focal Therapy
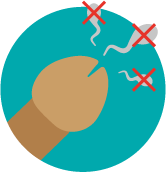
Focal therapies only target areas of your prostate that contain the most significant cancer.
These differ from whole gland therapies that involve treating the whole prostate gland for example, prostatectomy or radiotherapy.
Focal therapies are available in the UK:
Special arrangements are put in place by the National Institute for Health and Care Excellence (NICE) if there is a lack of long-term data on the effectiveness of a treatment. Before deciding on focal therapy, your healthcare team need to talk to you about:
NICE provides guidance on:
Learn more about NICE and what they do by visiting their website.

Informed consent is even more important for treatments under a special arrangement.
Informed consent means that you must be given all the information about:

Healthcare professionals who use focal therapies must collect information about:
This information may be:
They do not share information about individual patients.
‘Evidence suggests that this procedure is safe enough, but there is not enough evidence about how well it works. So, it can only be done with special arrangements. This means you will have regular appointments afterwards to check how well it is working or if it has caused problems’. NICE 5th April 2023.
For more information you can visit the NICE website (this link will open in a new external tab).
The statement from NICE on cryotherapy is similar to that for HIFU. For more information, you can read the NICE statement on cryotherapy (this link will open in a new external tab).
'There is not enough evidence about how well this procedure works in the long term. So, it can only be done with special arrangements. This means you will have regular appointments afterwards to check how well it is working or if it has caused problems..' NICE July, 2023.
For more information, visit the NICE website (this link will open in a new external tab).
Studies show these cancers can be effectively treated by focal therapy. However, there are a lack of randomised control trials comparing focal to whole gland treatments.
Randomised trials compare two or more different groups of patients. There is usually:
Randomisation is when people are put into either one of these groups by chance. A bit like flipping a coin. A computer decides which group you are in.
Randomisation is the best way of making sure that the results of trials are free from bias.
Visit our clinical trials page (this link will open in a new tab) for more information on how clinical trials work.
You may be able to have focal therapy if:
Your prostate cancer is contained within your prostate (localised prostate cancer) and your:
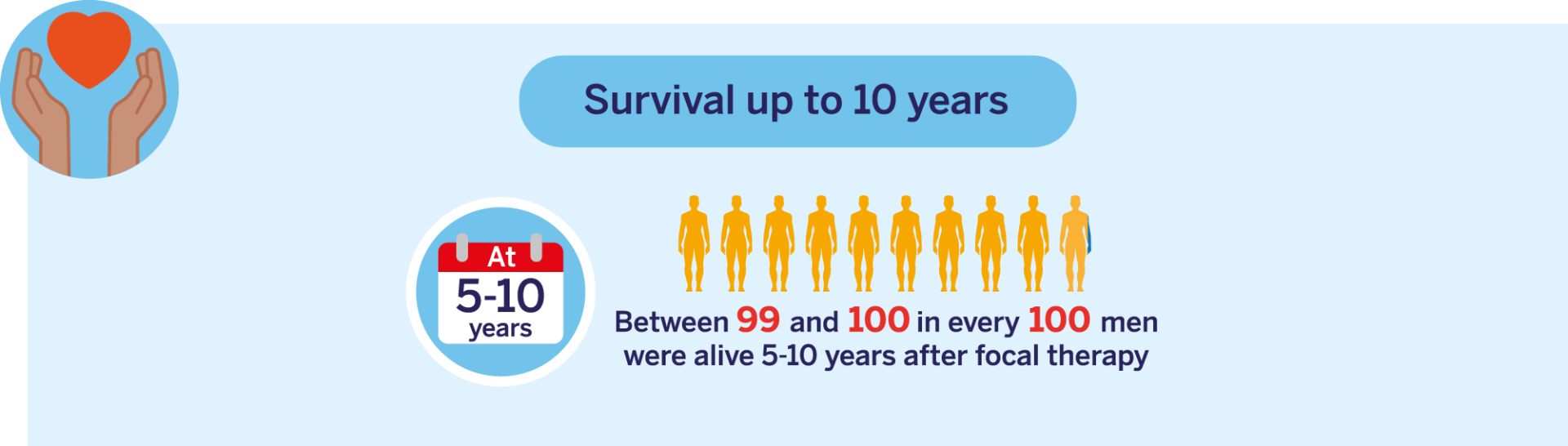
Please note: Data relates to cryotherapy and HIFU only.

Your doctor will look at the results of your:
They will then talk to you about all the treatments that are suitable for you. This will include the possible benefits as well as the risks and side effects. Your doctor and specialist nurse can support you to make a decision that is right for you and your lifestyle.

HIFU uses high intensity ultrasound waves to kill prostate cancer cells. This is done by heating the cancer cells to a high temperature. You will need a general anaesthetic.
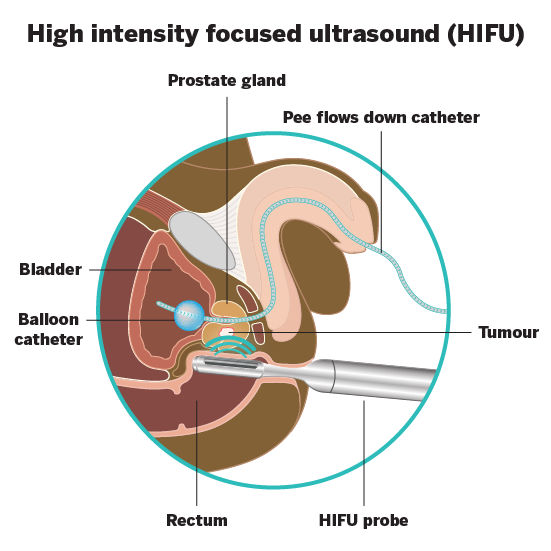
The whole procedure can take between 1 and 3 hours. This will depend on the size of the area that needs treatment.
Cryotherapy kills cancer cells by freezing them. It is done under a general anaesthetic.
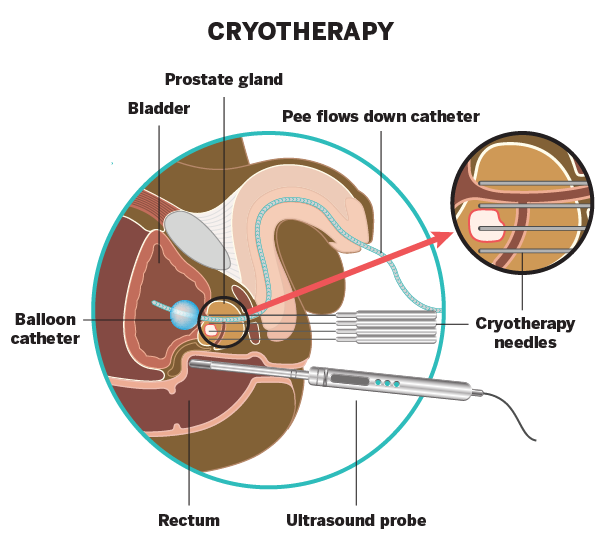
Your doctor will:
Irreversible electroporation uses electrical pulses to destroy cancer cells. It is done under a general anaesthetic.
Your doctor will pass:
The needles will be taken out at the end of the treatment.

What happens on the day of my treatment?
Your surgeon will visit you to:
Your anaesthetist who will ask you questions about:
You may be asked to wear a pair of compression stockings. These are sometimes called TED stockings. You may also have a heparin injection. This helps to thin your blood. Both help to stop blood clots (deep vein thromboses) forming in your lower legs.

You will have a tube to drain pee from your bladder into a bag. This is called a urinary catheter. A nurse will show you how to care for the
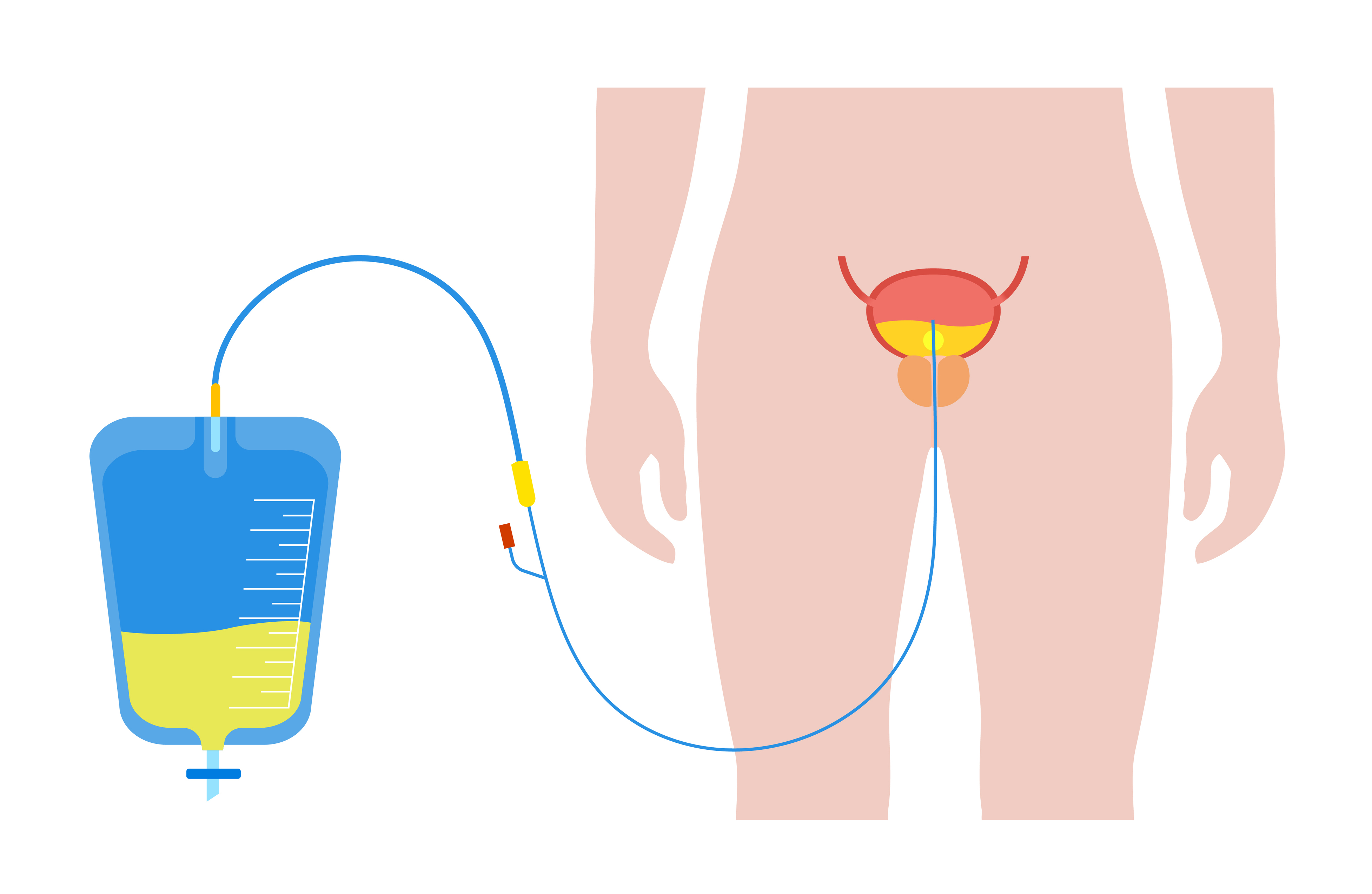
catheter.
You may have some pain in your penis and back passage. Your healthcare team will talk to you about painkillers.
It is the responsibility of the doctor who treated you to arrange a suitable follow-up plan. This may include regular PSA tests, MRI scans and prostate biopsies. Ask your doctor about what tests you will need after your treatment.
After your treatment, you will have your PSA levels checked:

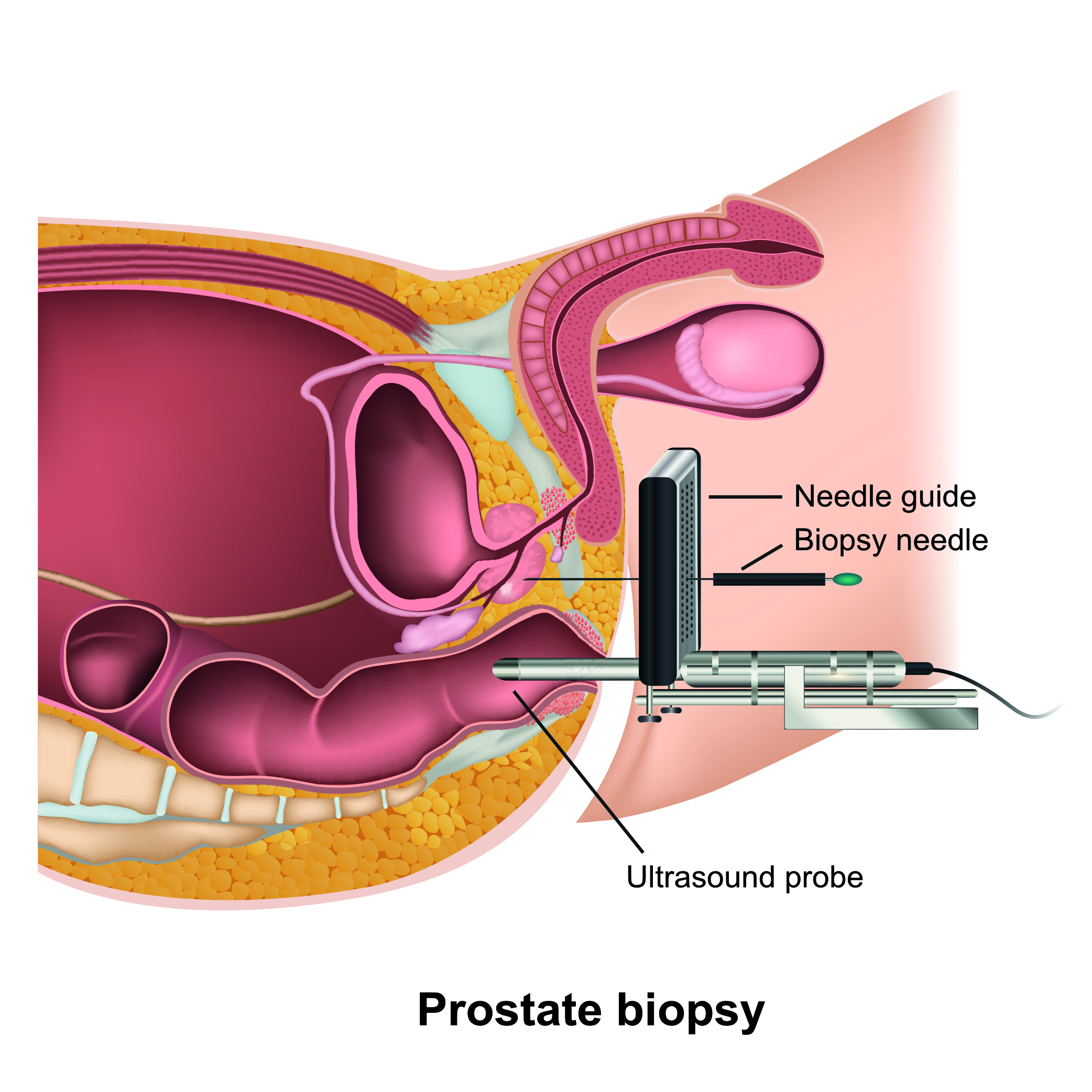
Visit our page on prostate biopsies to find out more.
If your cancer comes back, your doctor will talk to you about other treatments. The treatment you can have may depend on:
The treatments you have already had.
Possible treatments may include:


After 12 months
Between 1 in 100 and 2 in 100 people leaked pee.

The first 6 weeks after focal therapy
All men experience problems peeing due to the prostate healing.
After 12 months
5 in 100 people had problems peeing.
After 12 months
Less than 1 in 100 people had problems with their bowels.

Please note: All data relates to cryotherapy and HIFU only.
In the first 2-3 months
Most men will have problems getting or keeping an erection months and will need to use medication to help.
After 12 months
Between 5 in 100 and 20 in 100 people had problems getting or keeping an erection.
After 12 months
50 in 100 people had dry orgasms.
Please note: All data relates to cryotherapy and HIFU only.
Please note: All data relates to cryotherapy and HIFU only.
Enjoying activities such as walking or going out to the pub
57 out of 100
Ability to make good connections with others
21 out of 100
Ability to reach sexual arousal, either physically or emotionally
46 out of 100
Knowing who you are and what motivates you
25 out of 100
Feeling good and functioning well in your personal and professional life
39 out of 100
Ability to think clearly, make good decisions, and cope with your emotions
36 out of 100
Feeling of constant physical and/or mental tiredness or weakness
36 out of 100